Deciding What Matters: An Essentialist Model for Constraint-Led Resolution
Jarred Boyd PT, DPT, MSAT
In rehab and performance settings, we’re often taught to identify constraints - whether personal, task, or environmental - as the key influencers of movement. But rarely are we taught how to prioritize them. In practice, we don’t have the luxury of addressing every issue we’re faced with. Thus, it requires discernment: deciding what matters most, what’s modifiable, and what will create the greatest downstream effect. This is where an essentialist model becomes critical not to reduce complexity, but to filter it.
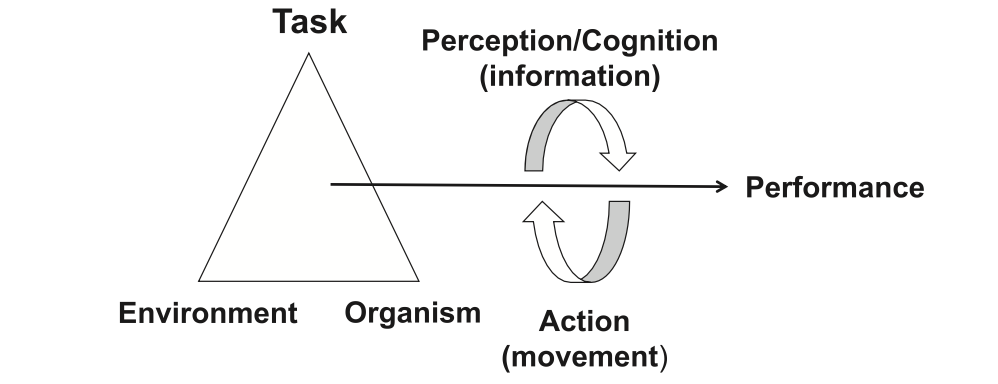
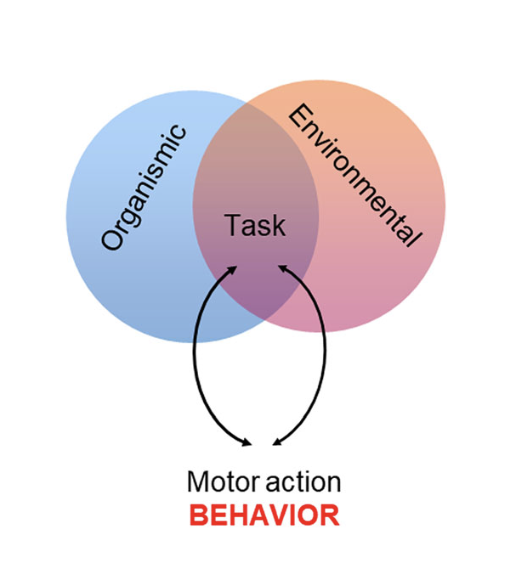
While the dynamic system of person level, task-level, and environment offers a conceptual entry point, we must go further: constraints are not just descriptors of behavior but instead they can be viewed as modifiable variables that influence load tolerance, capacity (kinetics), and movement expression (kinematics).
Guccione (2018)
In this sense, constraints can be considered moderators of injury risk or limiters of performance. But not all deserve intervention. The question isn’t just what’s present but rather what’s intervenable, relevant, and worth resolving.
Constraints as Load Moderators and Performance Filters
A helpful analogy: a load moderator functions much like a dimmer switch. It doesn’t generate mechanical load, just as a dimmer doesn’t produce electricity, but it can amplify, dampen, or regulate how much of that load is experienced by tissue. Person level, as denoted as internal constraints such as: force generating capacity, coordinative capabilities, etc. impact how forces are distributed across the musculoskeletal system. This is key: constraints don’t dictate deterministic movement behaviors, but they can influence the number of viable movement solutions available to solve a task – and as such, this may influence tissue specific loading.
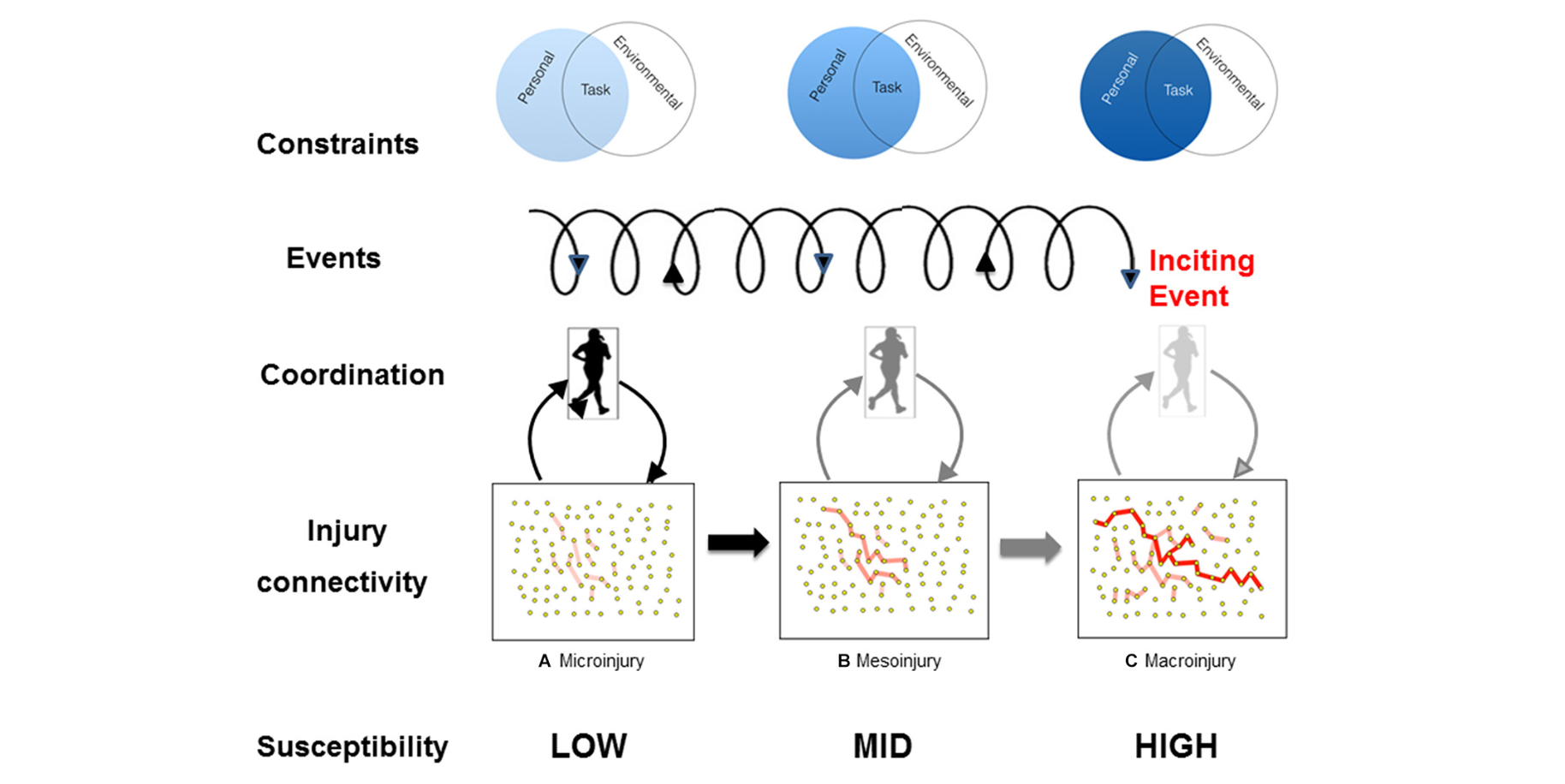
When tissues load threshold is surpassed, or mechanical fatigue failure occurs, the body often reduces variability in the affected region as a protective strategy. In response, the system may shift variability to other tissues or segments as a compensatory strategy, increasing their burden and potential for breakdown. This reflects the connectivity hypothesis (Pol et al., 2018), which suggests that the body responds to “instability” by reorganizing through synergy. While this can offer short-term coordination solutions if this reorganization is taxed repeatedly, the result capacity exceeding tissue thresholds leading to injury across different levels (micro, meso, macro).
Pol (2018)
Constraints, Affordances, and Movement Possibilities
Crucially, resolving constraints isn’t just about protecting the body it’s about expanding an athlete’s perceptual and behavioral bandwidth. As Balague and Pol (2019) describe, affordances are task-specific action possibilities that emerge from the relationship between the athlete and their environment. These are not static features of the world; they are scaled to the athlete’s action capabilities or better stated the - internal resources available to interact with the environment.
Balague (2019)
But herein lies a critical issue: there can be a mismatch between what is perceived and what can be executed. At times, an athlete may attempt to exploit an affordance such as a deceleration or an evasive maneuver but lack the force-generating capacity, tissue-specific strength, or impulse bandwidth to execute the task safely or effectively. In these cases, perception-action coupling breaks down. The athlete either fails to accomplish the task or compensates in a way that increases mechanical failure.
This is where internal constraints become both performance limiters and injury moderators.
Take, for instance, a basketball player attacking downhill who perceives the opportunity to decelerate and create separation for a step-back three. That movement depends on their ability to rapidly generate braking force. If they lack the constituents that underpin deceleration impulse capacity, an internal constraint, then:
The movement may not be perceived at all (it’s not an affordance in their landscape),
It may be perceived but not executed, or
It may be attempted and fail, overloading tissue that lacks the required readiness
In this scenario, the absence of a specific action capability filters out the affordance, shrinking the athlete’s movement landscape and limiting performance expression. This reinforces a key idea: affordances are not guaranteed by perception alone they must be underpinned by physical capabilities and capacities. When aforementioned is absent or misaligned with the perceived opportunity, the system becomes vulnerable.
Beyond enabling action, targeted physical preparation, particularly strength training derivatives, can also afford protection. These methods not only enhance performance by adapting the biomechanical and neuromuscular underpinnings of impulse, but also reduce the relative magnitude of stress-strain forces by improving tissue specific strength and distributing load more effectively. This protective affordance likely contributes to an expanded envelope of function, a theoretical construct describing tissue tolerance across a range of stressors, including variations in magnitude, duration, and direction. In this context, training serves to “inoculate” the musculoskeletal system, enhancing its capacity to attenuate external moments such as ground reaction forces and momentum.
Ultimately, the goal is to broaden the bandwidth of both tolerance and capacity, not just in what tissues can endure, but in the range of viable movement solutions the body can generate. This adaptability, or coordinative variability, allows athletes to move fluidly through fluctuating environments without aggregating mechanical stress and potentially failure onto a single structure. As Glazier (2021) notes the aim should not be the pursuit of “perfect” movement, instead the goal should be to develop a broad enough movement bandwidth to remain effective under changing task and environmental constraints, a principle that applies equally to performance and injury mitigation.
Constraint resolution, then, is not merely corrective it is a strategic re-expansion of movement potential and the distribution of variable stresses. More importantly, constraint resolution is about identifying which constraints, when resolved, create system-wide effects.
A Hierarchy of Need: What to Target First
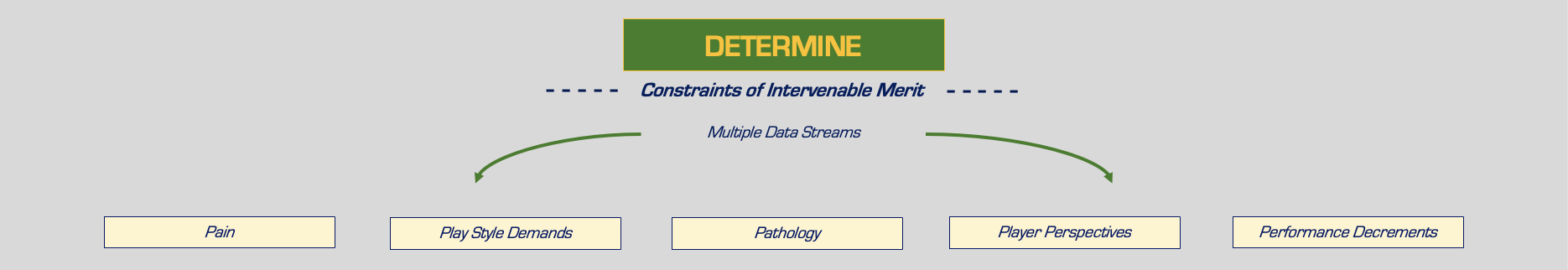
In my model, constraint resolution is filtered through five key lenses:
Pain
Play Style Demands
Pathology
Player Perspective
Performance Decrements
These aren’t isolated silos they form a sort of interacting map that helps determine which constraint is most relevant, most modifiable, and most likely to produce systemic change. I use a tiered model, drawing from both subjective input and objective data, to identify which constraint holds the most influence and is most modifiable in the current context. Often, resolving a single high-leverage constraint leads to downstream improvements in others.
This is about applying Occam’s razor to reconditioning: resolve the fewest things needed to unlock the largest systemic effect.
Occam’s Razor, often misunderstood as “the simplest answer is best,” is better framed as: “Entities should not be multiplied without necessity”. In other words, when two or more hypotheses are consistent with the available data, the one that introduces the fewest new assumptions should be preferred. This doesn’t mean the simplest answer is always correct but that every additional assumption introduces another point of failure, lowering the overall probability that a complex explanation is right.
This model is vital in rehab and performance, where uncertainty is inherent, but our decision-making still needs clarity. Too often, we fall into one of two traps:
Excessive complexity, where we over-layer inputs and variables without anchoring to first principles, paralyzing progress with overthinking.
Over-reductionism, where we isolate singular rudimentary causes (e.g., "weak glutes") and lose sight of the systemic interactions that matter.
Both extremes offer a false sense of certainty one dressed in intellectual complexity, the other in shallow reflection. Occam’s Razor offers a counter: simplify, but only with discernment. In the context of constraint resolution, it asks us:
What is the least amount we can intervene on to create a meaningful shift?
Which constraint is most likely to be causal, most modifiable, and least burdened by assumptions?
This forces us as clinicians to focus on high-probability levers, those that are both clinically relevant and logically sound, so that we don’t fall prey to chasing noise, stacking interventions, or clinging to overly elaborate frameworks.
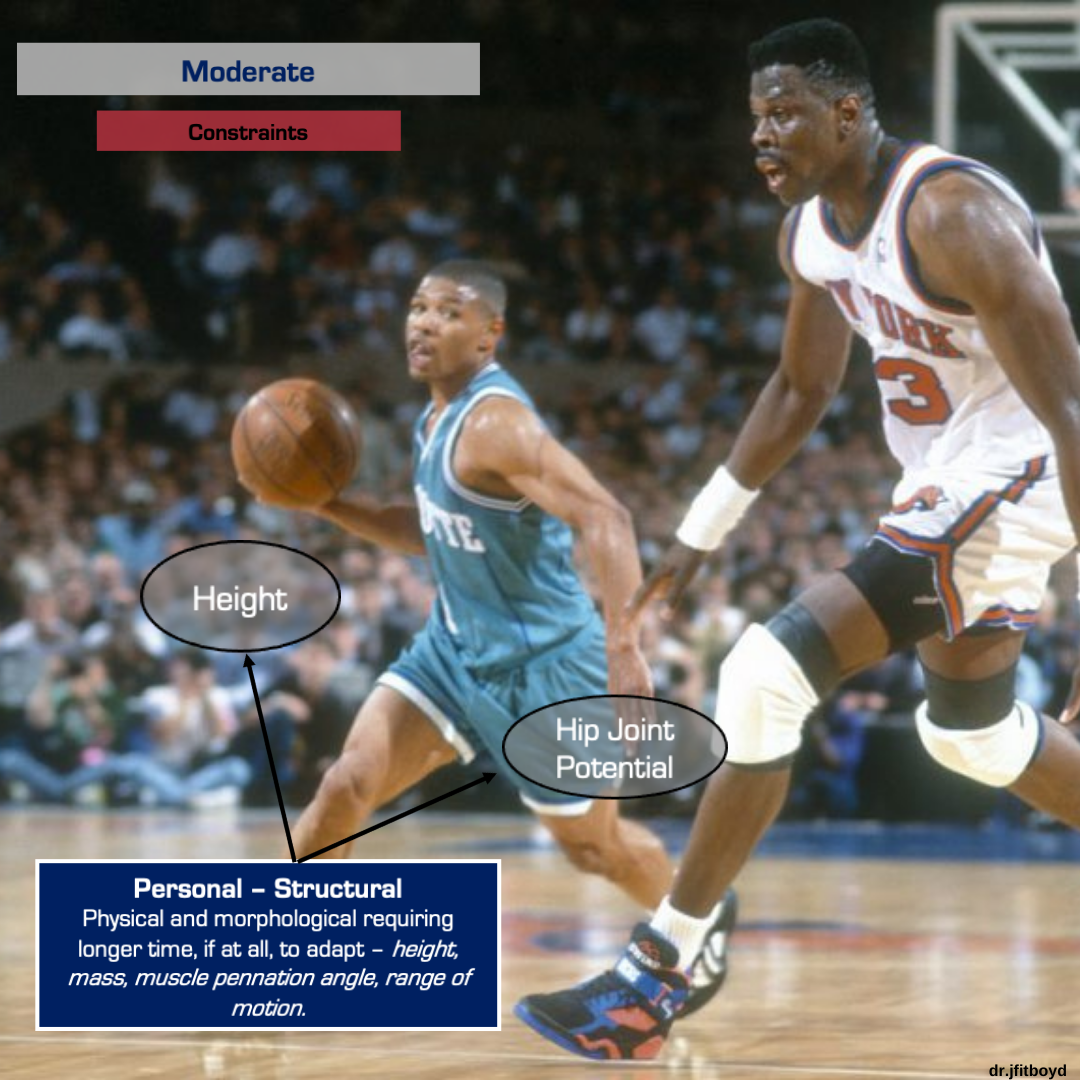
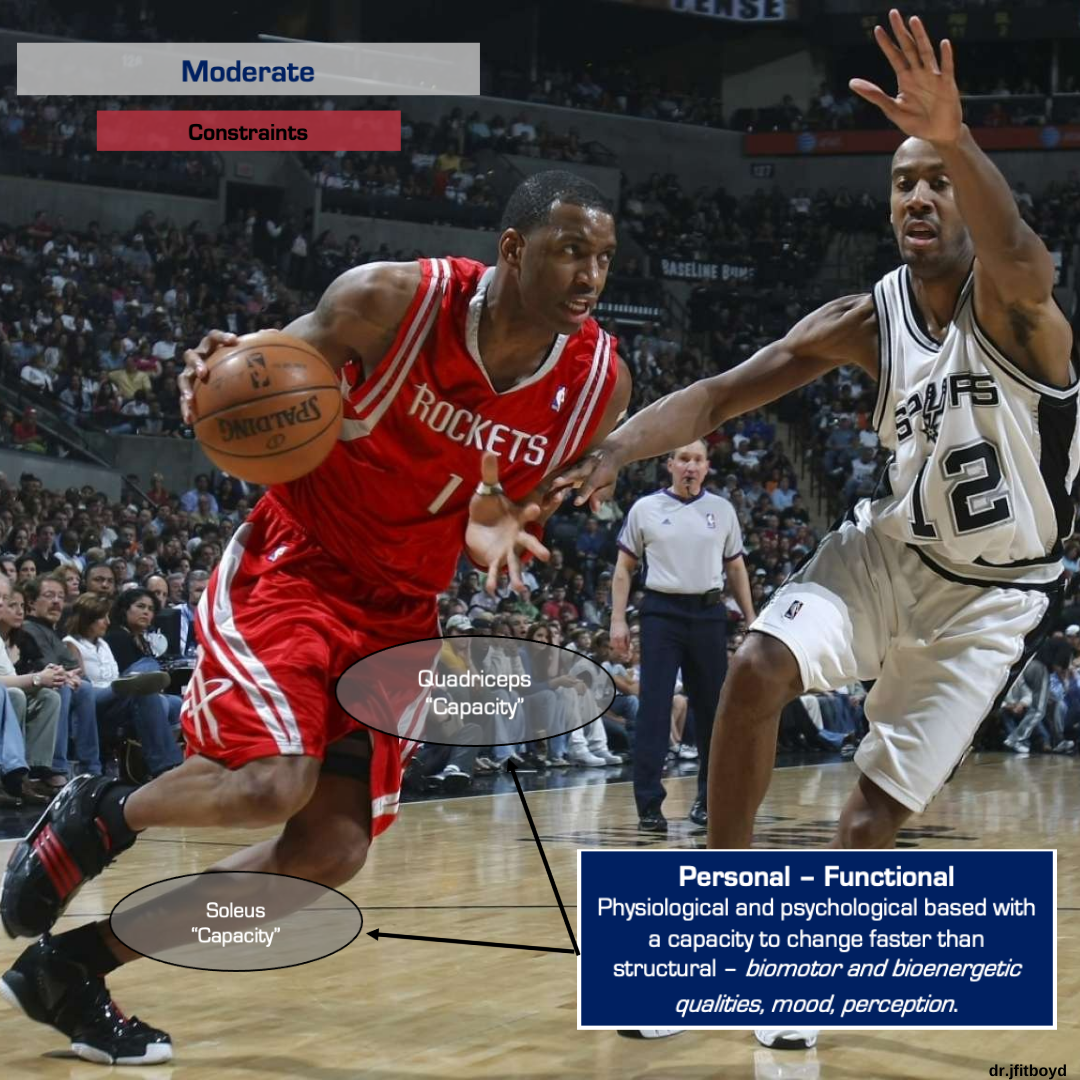
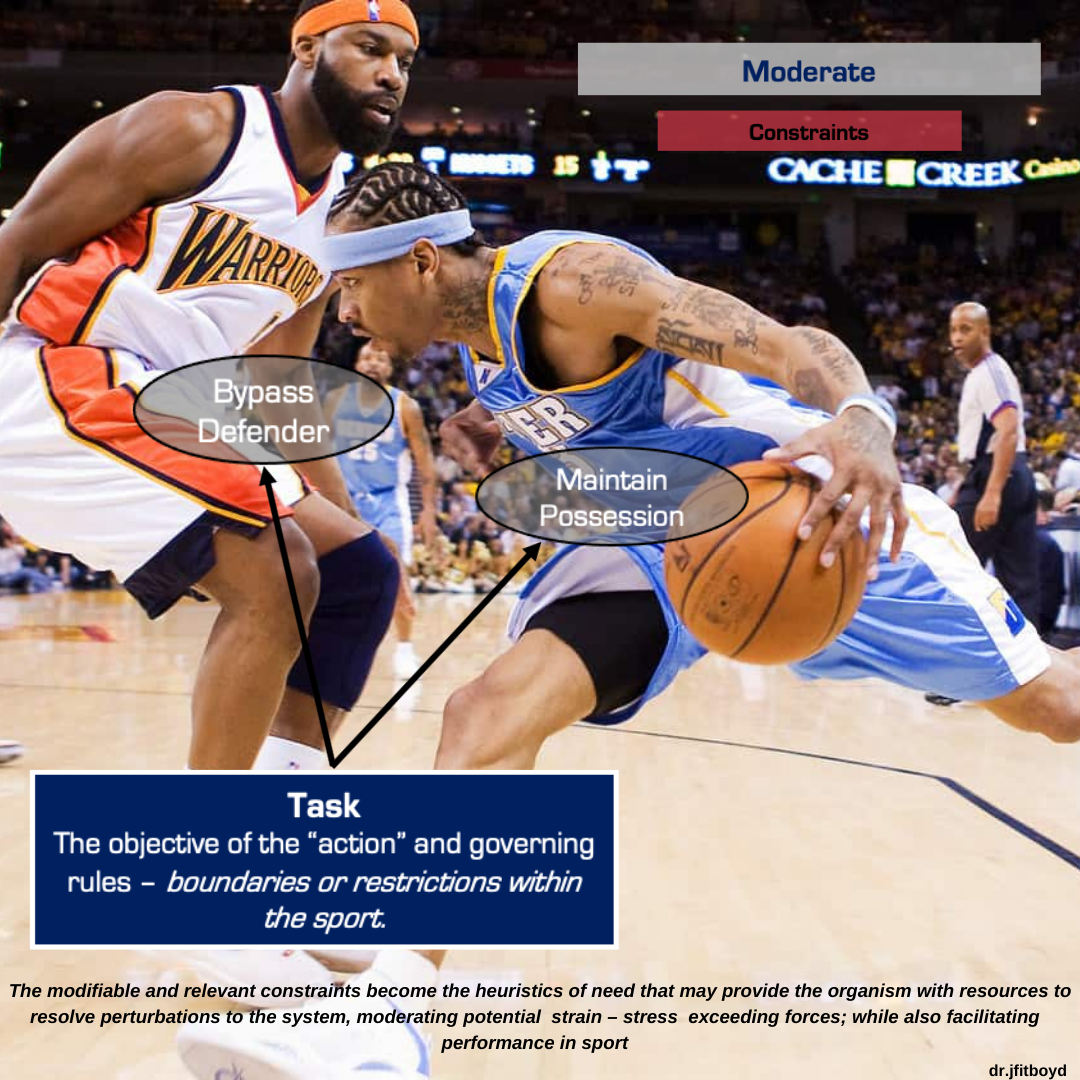
Practically, constraints can be categorized into (iterated from Glazier 2017):
Personal - Structural: anthropometrics, body composition, architecture (e.g., fascicle length) - adapting slowly.
Personal – Functional: strength, power, fatigue, rate of force development - more trainable.
Task-Related: interactions between athlete and sport-specific actions (e.g., defending or evading)
Environmental: surface, footwear, climate - modifiable in training but less so in live competition.
In my experience, personal, otherwise known as internal constraints - especially functional ones - are the most fruitful targets for expanding action capabilities and developing robustness. These are the levers that most directly influence an athlete’s ability to handle environmental variability, tolerate higher impulse demands, and adapt to shifting game scenarios.
The 5 Ps of Constraint Filtering: A Decision-Making Hierarchy for Complex Cases
1. Pain: A Bottleneck to Action
When pain enters the system, it often serves as an immediate bottleneck narrowing movement options, reducing variability, and shrinking the athlete’s affordance landscape. Whether acute or persistent, pain typically prompts the body to offload stress from the sensitized region. This isn’t inherently dysfunctional rather it can be viewed as an adaptive strategy. But when offloading becomes prolonged and unresolved, it can drive stress shielding, leading to reduced exposure to relevant mechanical loads and diminishing tissue tolerance over time.
This is where intentional mechanical (i.e. kinematic) positioning often comes into play. Early in rehab or during sensitization, mechanical alterations can be a useful temporary solution that helps redistribute load without overexposing a vulnerable tissue. Athletes should not be forced into these positions in purgatory; they're simply transitional affordances that buy time for graded reintroduction of stress. At this intersection, the concept of motor abundance becomes critically important.
Motor abundance refers to the blissful ability of the neuromuscular system to find multiple solutions to achieve a movement goal a natural consequence of redundancy and degeneracy. This degeneracy, where structurally different elements perform the same functions, is what gives humans adaptability, resilience, and “fluidity”. But in the context of pain, it becomes a double-edged sword. When a specific tissue or structure is no longer available to bear its usual load, the system will still solve the task but now at the expense of load-sharing elsewhere. The problem isn't the variability; it's the compensatory rigidity or fragility that emerges when movement solutions become constrained by pain. The system adapts, but not always at a sustainable rate.
Moreover, this isn’t just a biomechanical issue pain modulates how the athlete perceives and interacts with their environment. It influences what they notice, what they trust, and what they’re willing to do. This is where the concept of attunement is valuable. Attunement is the process by which an individual becomes increasingly sensitive to specifying informational variables, or cues, in the environment that signal opportunity for action (i.e., affordances). Pain can blunt this sensitivity. It narrows attention, biases perception toward threat, and can downregulate:
Impulse generation capacity
Coordinative variability
Trust in movement options
And while modern pain science rightly reminds us that pain does not equal tissue damage, this truth, when overemphasized, can create its own problem. It may lead us to dismiss mechanical contributors or subclinical overloads. Pain resolution is not synonymous with tissue restitution, but it may reflect improved exposure tolerance or early interception of brewing dysfunction.
Even when pathology isn’t visible, pain may still signal risk, reflecting altered force tolerance, neural sensitivity, or suboptimal load distribution – it’s not proof of damage, but neither is it meaningless. Clinically, niggles, those recurring low-grade symptoms, can serve as early warning signs. They often reflect a tissue ecology under strain: not yet pathological, but potentially trending toward overload. Research (e.g., Whalan et al. 2019) has shown that athletes reporting niggles have elevated risk for future time-loss injuries especially when those symptoms are ignored or poorly monitored. Pain, even subtle, filters our focus. It may not tell us exactly what to fix, but it often tells us where to begin our investigation.
2. Play Style Demands: The Tissue-Specific Signature of Movement
Every athlete brings a unique style of play, whether they’re a downhill attacker, a catch-and-shoot specialist, or a rim protector. These play styles aren’t just tactical labels, they ensue patterns of force exposure that have mechanical consequences for the body. In this model, play style serves as a filter that helps determine which constraints rise to the level requiring resolution.
This begins with a fundamental distinction:
Load refers to the external forces applied to the system such as: ground reaction forces, momentum, or joint torques.
Stress refers to the internal response of tissues to those loads, which is what muscles, tendons, cartilage, and bone actually experience.
And stress isn’t uniform. It varies depending on both tissue type and movement strategy:
Compressive stress, often driven by axial load, acts inwardly and can influence bone remodeling or articular cartilage health.
Tensile stress resists elongation is commonly experienced by muscle and tendon, and frequently implicated in hamstring or Achilles injuries.
Shear and torsional stress can emerge at joint interfaces or apophyseal regions when mechanical dissociation is limited.
Play style acts as a moderator for which tissues are exposed to which types of stress, and how frequently. Consider a rim runner, an athlete who thrives in transition and consistently reaches high sprint velocities. The repeated deceleration demands on the shank and posterior thigh create frequent exposure to eccentric braking forces. If this athlete presents with immature eccentric hamstring capacity, that becomes a meaningful internal constraint. It’s not just a deficit it’s a bottleneck that directly conflicts with their most relied-upon play style derived movement solution.
In this way, play style shapes which internal constraints are essential ingredients, not optional refinements. But force-generating capacity isn’t the only relevant constraint. Joint potential, particularly at diarthrodial joints, can meaningfully influence how stress is distributed during terminal tasks like braking, cutting, or defensive pivots.
Take an athlete with notably limited hip internal rotation. On paper, that might not warrant intervention. But if their developmental pathway includes becoming a high-level on-ball defender where rapid deceleration, cutting, and momentum arrestment are core to their identity - then that limitation may create compensatory strain elsewhere. For example, insufficient hip internal rotation may constrain segmental dissociation, thereby redirecting shear forces to the pubic joint during closed-chain deceleration actions.
This mechanical restriction may begin as benign but can accumulate toward subclinical overload over time. This doesn’t mean every limitation in joint ROM or force capacity must be resolved. Everyone has a relative movement bandwidth and chasing textbook ranges or idealized outputs in isolation often leads to diminishing returns and can be quite a futile endeavor. But when movement options are limited in ways that intersect with play style, they deserve closer scrutiny.
Play style doesn’t just reflect how an athlete moves it helps determine which constraints have systemic consequences if left unresolved. Thus, play style becomes a strategic filter:
It contextualizes constraint relevance
It bridges the mechanical and tactical layers of performance
It guides clinicians toward resolving the constraints that are not just present, but consequential
3. Pathology: A Marker of Tissue Viability, Not Just Symptom Expression
Pathology is often painted as black-and-white either present or absent, concerning or benign. But in practice, it’s far more ambiguous. As noted in Robbins & Cotran’s Pathologic Basis of Disease, pathology can be defined as “the study of the causes and effects of disease or injury, including the structural and/or functional deviations from ‘normal’ tissue anatomy and physiology.” Yet in the clinical setting, discerning the significance of a given pathology whether it warrants resolution or buffering is where the challenge lies.
That’s because pathology exists in abundance across the musculoskeletal system, often silently and without consequence. Degenerative disc changes, partial-thickness tendon tears, and labral abnormalities are well documented in asymptomatic populations. Their presence does not guarantee dysfunction, and their absence does not guarantee protection. But this shouldn’t excuse us from investigating their relevance. Two heuristics that help navigate the uncertainty, noise, and clinical gray area surrounding pathology is to consider:
Base rates of pathology within the sport or population, and
Prognostic data on the likely course or impact of that pathology if left unaddressed.
This is probabilistic thinking applied to constraint resolution - we’re not asking, “Is this pathology bad?” but rather, “What’s the likelihood it becomes meaningful under this athlete’s demands, history, and context?”
Take tendon pathology, for example. There is abundant literature demonstrating that structural changes to the tendon (e.g., hypoechoic regions, neovascularization) can exist independently of pain (Rio et al., 2014; Docking et al., 2015). Yet these changes may still influence tissue mechanics, motor coordination, or regional load-sharing, which as the connectivity hypothesis suggests, can provoke stress-strain in adjacent segments or systems over time.
Importantly, pain should not be the sole lens we use when assessing whether a pathological constraint deserves resolution. Performance limitations, be it in jump height, deceleration capacity, or change of direction capability, may also emerge from structural deficits, even when symptoms are absent.
Furthermore, pathology offers insight into a tissue starting point and long-term viability. While we can’t confidently “prevent” injury, understanding what tissue insult exists helps us estimate load-bearing tolerance and potential recovery bandwidth. In high-exposure sports like basketball where intensity and frequency of load exposure often exceed recoverable timelines these considerations become strategic. For example, a focal chondral defect in the knee may be asymptomatic but poses a clear risk to long-term joint health. For example, Kaplan et al. (2005) found that 47.5% of asymptomatic professional basketball players had MRI detected articular cartilage lesions. Given the limited reversibility of cartilage degeneration and the biological entropy that follows, this form of pathology may justify proactive intervention even if other constraints aren’t currently signaling distress.
This leads to an important question:
If pathology is present but there is no pain or performance decrement, is intervention still justified? This question sits at the heart of this model. The answer depends on how that pathology interacts with the other 5Ps:
Is it paired with pain?
Does it influence performance?
Does it align with the athlete’s perspective or concern?
Does their play style impose recurring stress onto that region?
These filters don’t operate in silos, instead they converge and interact amongst one another. And in doing so, they help determine whether a given pathology is worth resolving now, or simply worth monitoring. We must also consider the second-order consequences of acting or not acting. If the pathology is clinically silent but would require invasive correction, do the potential downsides outweigh the upside? Conversely, if the athlete’s play style continually exposes that area to high strain, the risk–benefit analysis may shift in favor of proactive constraint resolution.
4. Player Perspective: Contextualizing the Data and Closing the Gaps
Objective performance testing is essential, from force diagnostics, motion capture and jump profiles all help illuminate where deficits may lie. But equally important is intentionally analyzing the game itself and deliberately discussing the athlete’s perspective. It’s in this integration of data and lived experience that we increase the probability of identifying the most meaningful, trainable rate limiters.
While pain, pathology, performance decrements, and play style demands all serve as valuable filters, they tend to bias toward the quantitative, observable, and externally framed. What’s often missing is the subjective filter the athlete’s own experience of their body, movement, and limitations. And that lived experience often holds signals that are just as powerful sometimes more potent than what force plate, for instance, tells us.
In the context of internal load monitoring, RPE (Rate of Perceived Exertion) has been shown to rival, and at times outperform, objective markers in predicting readiness, recovery, and risk. That alone should shift how we value the athlete’s perspective - not as anecdotal “soft data,” but as an essential, perhaps required, input.
With this in mind, why not apply the same logic to constraint resolution?
Incorporating the athlete’s perspective allows us to test our hypotheses against their reality. It’s a means of verifying whether the constraints we identify as clinically relevant actually align with what the athlete perceives as meaningful or limiting.
Incorporating the athlete’s perspective allows us to:
Compare our hypotheses against their reality
Cross-check whether what we believe is a priority aligns with what they feel is holding them back • Uncover hidden rate limiters that may not yet show up in the metrics
This becomes especially critical when we begin prescribing interventions. Once we determine what constraint is most worth resolving we then describe the strategy meant to address it. But that intervention is only as impactful as the athlete’s willingness to engage with it. And engagement is often dictated by how well the intervention narrative resonates with their internal landscape their goals, fears, confidence, and experience. If there’s a mismatch between what we’re targeting and what the athlete believes is holding them back, even the most well-designed intervention will be irrelevant.
Technology has exponentially advanced our understanding of external loads, movement profiles, and force generating capacities. But for all its power, technology is not omniscient. There are still known unknown’s, variables we recognize but can’t fully capture, and unknown unknown’s factors, outside the current scope of measurement. The athlete’s perspective helps bridge those gaps. Not by giving us more numbers but by giving us context. Ultimately, the point is not to choose between objective testing and subjective input it’s to connect them. One gives us the “what while the other gives us the “why.”
5. Performance Decrements: When Kinetics Become Constraints
Performance decrements, particularly in the kinetic and strength domains, often act as large-scale constraints, limiting an athlete’s ability to solve movement problems under load and increasing their susceptibility to both instantaneous and accumulated stress-strain exposures. In this context, I defined strength as task-specific iterations of force over varying timescales. These include the magnitude and rate of force production required to reverse the downward acceleration of the center of mass, decelerate momentum (mass × velocity), or generate the high-impulse outputs necessary for locomotive directional changes. When these kinetic underpinnings are underdeveloped or degraded, they become potential bottlenecks to both safety and success, moderating the stress and strain experienced by tissue under high-demand actions.
However, performance limitations rarely present as a single failing on a single test. More often, they emerge as a triangulated pattern visible across isolated, integrated, and dynamic assessments. For instance, a reduced eccentric knee extensor capacity measured via isokinetic dynamometry may be the isolated manifestation of a broader issue. That same athlete may underperform on an eccentric single-leg leg press or display asymmetrical load capacity in a rear-foot elevated split squat each revealing a more integrated layer of the deficit. Dynamically, this same constraint could express itself as asymmetry in eccentric deceleration impulse during a countermovement jump. Peeling back the layers in this way allows us to trace the decrement from the clinical table to the chaos of play ensuring our interventions are grounded in context.
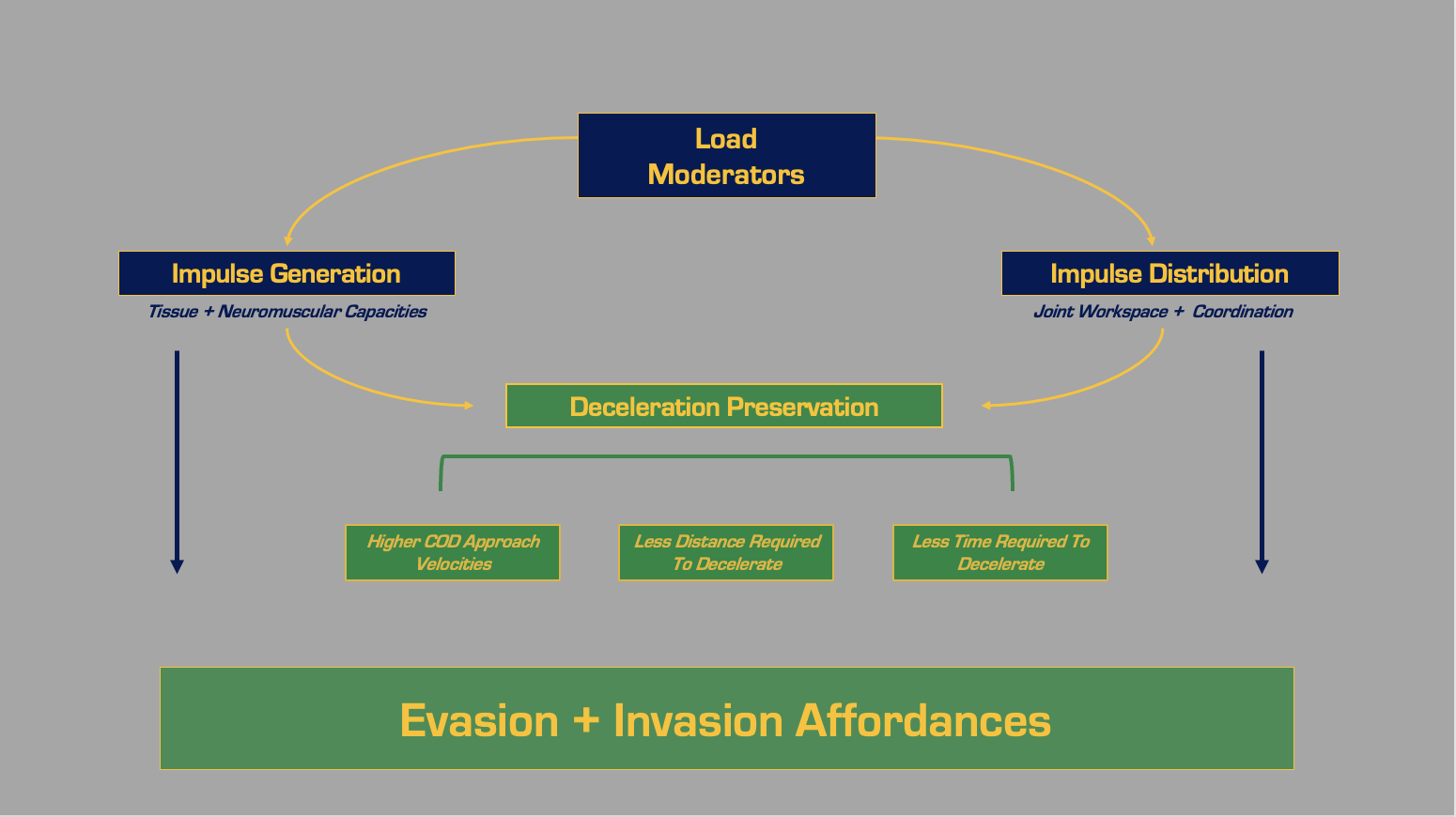
These kinetic constraints both in impulse generation are foundational to an athlete’s ability to exploit the affordance landscape.
Impulse generation – the neuromuscular and tissue capacity to produce force.
Impulse distribution – the coordination and joint workspace needed to apply that force effectively.
Invasion and evasion strategies, for example, rely on the body’s ability to coordinate force across time and space. Any reduction in either force output or joint-specific coordination may not only reduce performance but also disrupt stress distribution, potentially leading to structural overload. This interplay becomes even more relevant when viewed through the lens of play style. Consider a guard whose success depends on their ability to create space through separation. The task of stopping on a dime to execute a step-back three, or to decelerate and reaccelerate in a different direction, is highly dependent on robust braking impulse. If that athlete exhibits decrements, whether isolated, integrated, or dynamic, their potential becomes constrained, not only in terms of output but in available movement solutions.
Critically, identifying a performance decrement does not tell us what to do next. It raises a flag, signaling the need to investigate further and determine the constraint behind the constraint. Is the limiting factor neurological such as impaired motor unit recruitment or rate of motor unit recruitment? Or is it biological perhaps tied to contractile cross-sectional area, pennation angle, or fascicle length? These questions guide us toward the root of the limitation, but in the context of this model, the immediate focus is to assess whether that decrement rises to the level of essentialism: is it one of the vital few constraints that, when addressed, affords protection and augments performance?
This is the essence of targeted reconditioning, distilling signal from noise, and designing inputs that engineer both action capabilities and tissue resilience. When the right decrement is resolved, the downstream payoff can be greater than the localized gain. By augmenting the constituents of impulse, we can expand the movement bandwidth, reinforce the tissue scaffolding, and unlock affordances that were previously unavailable. That is how constraint resolution contributes not just to performance expression, but to long-term durability.
Conclusion: Choosing the Right Constraint to Resolve
Most athletes, regardless of their impressive athletic prowess and awe-inspiring feats, possess a bevy of internal constraints. But time is finite, and urgency is always pressing in high performance sport settings. As such, it is imperative that practitioners learn to discern which constraints are most essential. As we’ve seen throughout this model, that decision is guided by mental models like probabilistic thinking and second-order consequences. We are attempting to hedge our bets using both objective data and contextual insight to identify which constraint, when resolved, is most likely to augment performance or afford protection. But just as important is the flip side of that equation: What are the downstream consequences if we don’t resolve the constraint? Will the lack of action allow a meaningful degradation of tissue capacity, performance expression, or resilience?
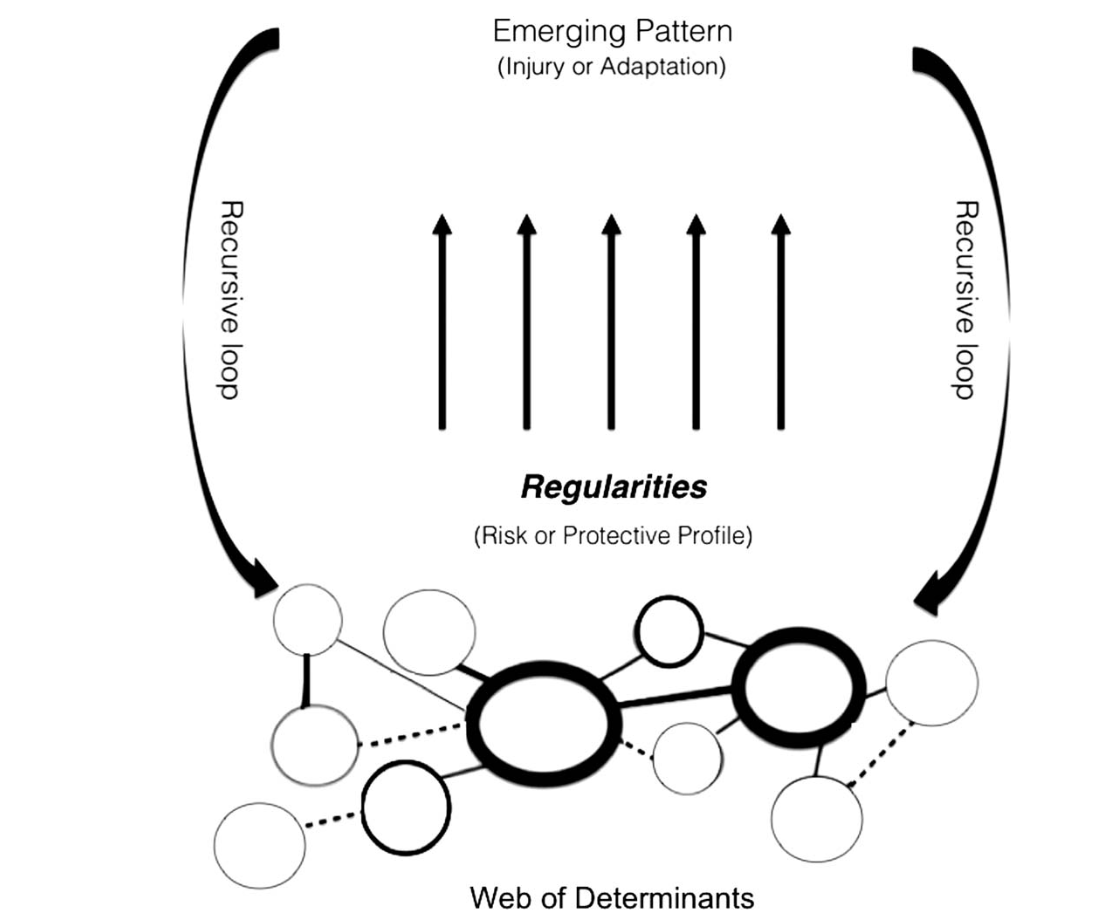
Bittencourt (2016)
At first glance, constraints may appear analogous to risk factors variables that limit the range of viable solutions and reduce performance potential. But we should aim to view constraints through a more systems oriented lens as part of a web of determinants (Bittencourt et al., 2016), rather than isolated red flags. Risk factors are not stand-alone variables they often emerge as constraints arising from multiple interacting systems. These patterns may reduce the system’s ability to tolerate stress, contend with impulse demands, or redistribute loads across tissues.
This is precisely why the 5 Ps framework can be so powerful. It reveals how constraints can exist across multiple domains, biological, perceptual, mechanical, tactical, and are often interconnected. Instead of relying on linear cause-effect chains, we begin to see patterns of interaction. We begin to prioritize the constraint that perturbs the system most meaningfully. Simply having a risk factor or constraint does not guarantee injury or underperformance. The context, the system, and the relationships between constraints matter far more than any single input.
This perspective invites us to think deeply not just about variables, but about relationships, interactions, and emergent properties. Constraints are not merely limitations; they shape action capabilities. And action capabilities, in turn, shape the affordance landscape an athlete can access.
Decision-making, especially under uncertainty, is never easy. We are often buried under an avalanche of information. The stakes are high, time is limited, and the reversibility of certain choices is low while the consequentiality can be high. My hope is that this model, the 5 Ps, offers a practical, scalable map. One that helps us navigate complexity with clarity, and filter signal from noise as we decide what to resolve, and more importantly, why.
References
Balagué, N., Pol, R., Torrents, C., Ric, A., & Hristovski, R. (2019). On the Relatedness and Nestedness of Constraints. Sports Medicine - Open, 5(6). https://doi.org/10.1186/s40798-019-0178-z
Bittencourt, N. F. N., Meeuwisse, W. H., Mendonça, L. D., Nettel-Aguirre, A., Ocarino, J. M., & Fonseca, S. T. (2016). Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition—narrative review and new concept. British Journal of Sports Medicine, 50(21), 1309–1314. https://doi.org/10.1136/bjsports-2015-095850
Docking, S. I., Ooi, C. C., & Connell, D. (2015). Tendinopathy: Is Imaging Telling Us the Entire Story? Journal of Orthopaedic & Sports Physical Therapy, 45(11), 842–852. https://doi.org/10.2519/jospt.2015.5880
Glazier, P. S. (2017). Towards a Grand Unified Theory of sports performance. Human Movement Science, 56, 139–156. https://doi.org/10.1016/j.humov.2015.08.001
Guccione, A. A., Neville, B. T., & George, S. Z. (2018). Optimization of Movement: A Dynamical Systems Approach to Movement Systems as Emergent Phenomena. Physical Therapy, 99(1), 3–9. https://doi.org/10.1093/ptj/pzy116
Kalkhoven, J. T., Watsford, M. L., & Impellizzeri, F. M. (2020). A conceptual model and detailed framework for stress-related, strain-related, and overuse athletic injury. Journal of Science and Medicine in Sport, 23(8). https://doi.org/10.1016/j.jsams.2020.02.002
Kaplan, L. M., Schurhoff, M. R., Selesnick, H., Thorpe, M., & Uribe, J. W. (2005). Magnetic Resonance Imaging of the Knee in Asymptomatic Professional Basketball Players. The Journal of Arthroscopic and Related Surgery, 21(5), 557–561. https://doi.org/10.1016/j.arthro.2005.01.009
Pol, R., Hristovski, R., Medina, D., & Balague, N. (2018). From microscopic to macroscopic sports injuries. Applying the complex dynamic systems approach to sports medicine: a narrative review. British Journal of Sports Medicine, 53(19), 1214–1220. https://doi.org/10.1136/bjsports-2016-097395
Rio, E., Kidgell, D., Purdam, C., Gaida, J., Moseley, G. L., Pearce, A. J., & Cook, J. (2015). Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British Journal of Sports Medicine, 49(19), 1277–1283.
About The Author
Jarred Boyd PT, DPT, MSAT
Sports Certified Specialist
Certified Strength Conditioning Specialist
Director of Rehabilitation Memphis Grizzlies
Jarred Boyd is the Director of Rehabilitation for the Memphis Grizzlies, where he operates at the intersection of performance, clinical practice, and return-to-play strategy. A Doctor of Physical Therapy with a systems-thinking approach, Jarred integrates biomechanics, tissue-specific adaptation, and neuromuscular diagnostics to solve complex reconditioning challenges. His work is grounded in first-principles thinking and guided by decision-making models that prioritize tissue health without sacrificing sport-specific readiness. He’s contributed thought leadership to platforms like The Science PT and continues to explore how signal, structure, and context shape adaptive outcomes in elite sport.